Inflammatory Bowel Disease: Symptoms, Causes, Diagnosis, and Treatment
Inflammatory Bowel Disease, commonly known as IBD, is a chronic condition that includes two main disorders: Crohn’s disease and ulcerative colitis. Both cause long-term inflammation of the digestive tract, leading to symptoms such as abdominal pain, diarrhea, and the presence of blood in stool. Although IBD has no permanent cure, modern treatments can help control inflammation, reduce flare-ups, and maintain remission for extended periods.
What Is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease (IBD) refers to a group of conditions characterized by continuous inflammation of the gastrointestinal (GI) tract. This inflammation disrupts normal digestion and nutrient absorption and often leads to cycles of flare-ups (when symptoms worsen) and remission (when symptoms subside).
IBD doesn’t only affect the intestines—it can impact a person’s overall health, influencing emotional well-being, nutrition, and quality of life. Though lifelong, the disease can often be managed successfully with medical care and lifestyle changes.
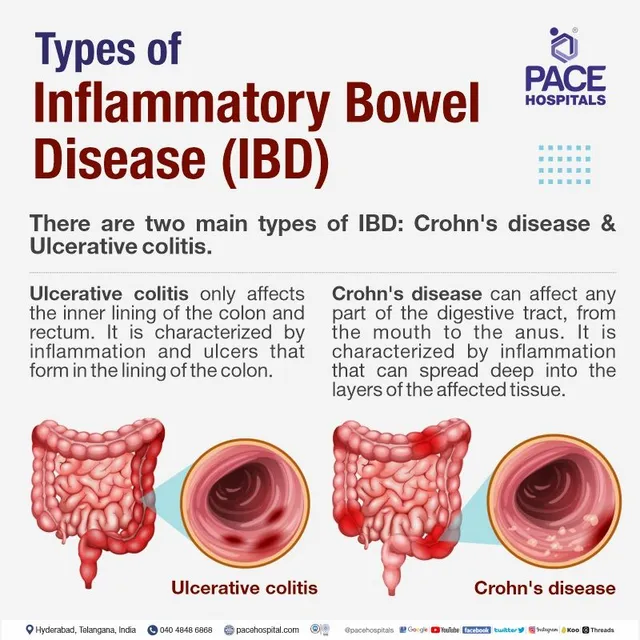
Types of Inflammatory Bowel Disease
There are two main types of inflammatory bowel disease:
- Crohn’s Disease:
This type can affect any part of the digestive tract, from the mouth to the anus, though it most commonly involves the small intestine and the beginning of the large intestine. Crohn’s disease causes deep inflammation and ulceration that may extend through multiple layers of the intestinal wall. - Ulcerative Colitis (UC):
Ulcerative colitis affects only the large intestine (colon) and rectum. It causes continuous inflammation and ulcers on the inner lining of the colon, leading to bleeding and discomfort.
How Common Is Inflammatory Bowel Disease?
It is estimated that about 1.6 million people in the United States live with some form of IBD. The condition can develop at any age, but it’s most frequently diagnosed between ages 15 and 35. Both children and older adults can also be affected.
Symptoms and Causes of Inflammatory Bowel Disease
Common Symptoms of IBD
Symptoms vary in severity and can appear suddenly or gradually. Periods of intense symptoms are referred to as flares, while symptom-free phases are called remission. Common signs and symptoms include:
- Cramping or pain in the lower abdomen
- Persistent diarrhea
- Blood in the stool
- Fatigue or tiredness
- Unexplained weight loss
During flares, these symptoms can become severe enough to interfere with daily life and may require medical attention.
What Causes Inflammatory Bowel Disease?
The exact cause of IBD remains unclear, but research suggests that it develops due to an abnormal immune system response. Normally, the immune system protects the body from harmful bacteria and viruses. In IBD, immune cells mistakenly attack healthy cells in the intestines, triggering inflammation.
Several factors may contribute to this immune malfunction, including:
- Genetic mutations: More than 160 “susceptibility genes” have been linked to IBD.
- Immune system dysregulation: The immune system becomes overly active or fails to turn off appropriately.
- Intestinal barrier issues: Damage to the gut lining may allow bacteria to enter tissue and cause inflammation.
- Gut microbiome imbalance: Changes in intestinal bacteria may increase inflammation risk.
Common triggers that may worsen symptoms include:
- Use of antibiotics or nonsteroidal anti-inflammatory drugs (NSAIDs)
- Smoking
- High stress levels
- Infections
Does Food Affect Inflammatory Bowel Disease Symptoms?
Food itself does not cause IBD, but certain foods or drinks can worsen symptoms during a flare. Each person’s triggers are different, but common culprits include:
- Alcoholic beverages
- Caffeinated or carbonated drinks
- Dairy products
- Foods high in fat or fiber
- Fried or greasy foods
A dietitian can help identify and avoid foods that trigger symptoms.
Risk Factors for Developing Inflammatory Bowel Disease
The strongest known risk factor is a family history of the condition. Studies suggest that 5–20% of people with IBD have a parent, sibling, or child who also has it. Other possible risks include certain infections, environmental exposures, and smoking.
Possible Complications of Inflammatory Bowel Disease
IBD can cause complications within and beyond the digestive system, including:
- Colon cancer: Long-term inflammation increases colon cancer risk.
- Perforated bowel: A hole in the intestinal wall can cause severe abdominal pain and requires emergency treatment.
- Toxic megacolon: Dangerous swelling of the colon that can be life-threatening.
- Anal fistulas and stenosis: Painful complications affecting the anal canal.
Other health issues linked to IBD include:
- Anemia (low red blood cell count)
- Blood clots
- Joint inflammation
- Eye irritation
- Mouth sores
- Liver disease
- Kidney stones
- Skin rashes or ulcers
- Osteoporosis due to nutrient malabsorption
Diagnosis and Tests for Inflammatory Bowel Disease
How Is IBD Diagnosed?
Diagnosis begins with a physical exam and a detailed review of medical history and symptoms. Healthcare providers may recommend several diagnostic tests, such as:
- Blood tests: To check for anemia, infection, or inflammation
- Stool tests: To detect blood or infection
- Colonoscopy: To view the colon and collect tissue samples (biopsy)
- Flexible sigmoidoscopy: To examine the rectum and lower colon
- CT or MRI scans: To assess inflammation in deeper tissue layers
- Capsule endoscopy: Swallowing a camera capsule to view the small intestine
- Upper endoscopy: To examine the esophagus, stomach, and small intestine
These tests help confirm the type and extent of IBD and rule out other digestive disorders.
ALSO VISIT
Management and Treatment of Inflammatory Bowel Disease
How Is IBD Treated?
While IBD cannot be cured, treatment focuses on reducing inflammation, relieving symptoms, and maintaining remission. Treatment strategies often include medications, lifestyle modifications, and sometimes surgery.
1. Medications
Doctors may prescribe one or more of the following types of medication:
- Anti-inflammatory drugs (corticosteroids): Help reduce active inflammation.
- Immunosuppressants or immunomodulators: Regulate or suppress immune activity to prevent attacks on the intestine.
- Biologic therapies: Target specific immune molecules responsible for inflammation.
- Antibiotics: Used if infections occur, particularly with abscesses or fistulas.
- Antidiarrheal medications: Control frequent bowel movements during flares.
2. Surgery
If medication fails to control symptoms or complications develop, surgery may be necessary. Surgical options include removing damaged sections of the intestine (colectomy) or creating new pathways for waste elimination. Surgery can often lead to long-term remission.
Prognosis and Long-Term Outlook
IBD is a lifelong condition that requires continuous management. Regular follow-ups with healthcare providers are crucial to monitor inflammation and prevent complications.
Even during remission, patients are encouraged to schedule checkups every 6 to 12 months, with more frequent visits during flares. Because IBD increases the risk of colon cancer, screening colonoscopies often begin earlier and occur more frequently than in the general population.
Living with IBD
Self-Care Tips
Living with IBD can be unpredictable, but these strategies may help improve quality of life:
- Monitor your diet: Identify foods that worsen symptoms and avoid them.
- Stay hydrated: Chronic diarrhea can cause dehydration.
- Keep an emergency kit: Include spare clothing, wipes, and tissues.
- Track symptoms: Keeping a journal can help identify triggers.
- Manage stress: Stress management techniques such as yoga, meditation, or therapy can reduce flare-ups.
- Seek support: Join support groups or connect with others living with IBD.
- Quit smoking: Smoking is a major trigger for Crohn’s disease.
- Consider mental health support: Counseling or therapy can help manage the emotional impact of chronic illness.
When to Consult a Healthcare Provider
You should contact your provider if you experience:
- Persistent or worsening abdominal pain
- Blood in stool
- Severe diarrhea that does not improve
- Unexplained weight loss
- New or severe fatigue
Emergency Situations to Watch For
Go to the emergency room or call emergency services if you experience:
- High fever or chills (above 100.3°F / 37.9°C)
- Severe abdominal swelling or pain
- Continuous vomiting
- Heavy rectal bleeding or blood clots in stool
These may be signs of serious complications such as toxic megacolon or intestinal perforation.
Summary: Understanding IBD
Inflammatory Bowel Disease (IBD) is a complex, lifelong condition requiring ongoing medical care and personal management. With proper treatment, lifestyle adjustments, and support, most people with IBD can lead active, fulfilling lives.