Heart Disease: Types, Causes, and Symptoms
Heart disease encompasses a variety of conditions that impact how the heart functions. Also referred to as cardiovascular disease, it includes not only heart-related issues but also diseases affecting blood vessels. In the United States, heart disease is the leading cause of death, accounting for around 700,000 fatalities annually—roughly 1 in every 5 deaths.
Each form of heart disease presents with its own set of symptoms and treatment options. Some conditions can be managed effectively with medication and lifestyle adjustments, while others may require surgical intervention.
Below is an in-depth look at the different types of heart disease, their causes, symptoms, and how they are diagnosed and treated.
Understanding Heart Disease Types, Causes, and Symptoms
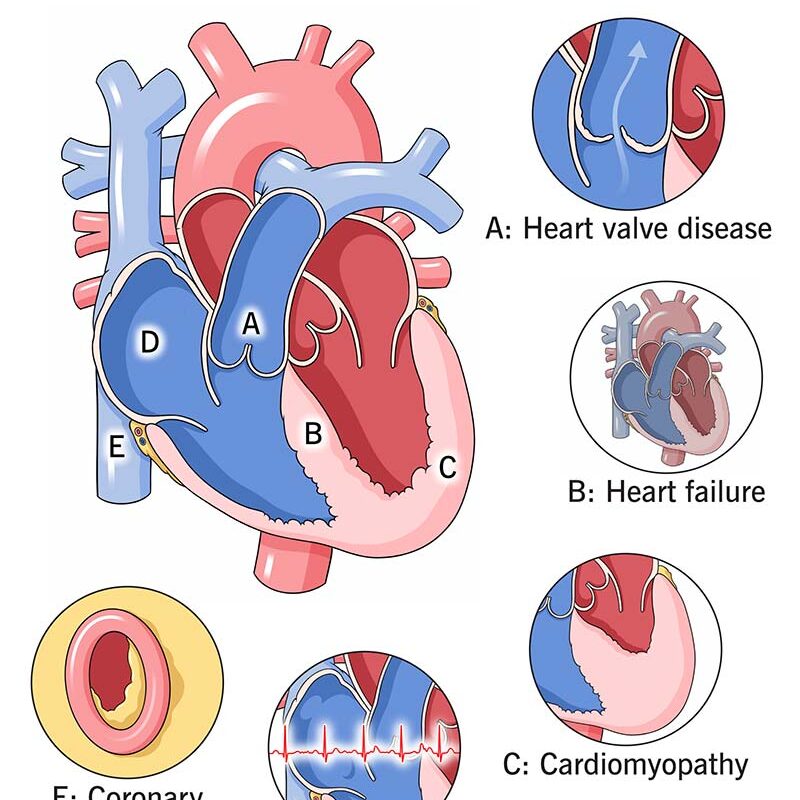
Heart disease can involve any part of the heart or blood circulation system. This includes:
Arteries supplying blood to and from the heart
Heart valves regulating blood flow within the heart
The heart muscle itself
The pericardium (a sac surrounding the heart)
- Coronary Artery Disease (CAD)
What It Is:
CAD is the most widespread and deadly form of heart disease. It occurs when the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked due to plaque buildup—a condition called atherosclerosis.
What It Causes:
Reduced oxygen flow to the heart
Chest pain (angina)
Increased risk of heart attacks
Potential complications like arrhythmias or heart failure
Risk Factors:
Age (Men over 55, women post-menopause)
Lack of physical activity
Diabetes or metabolic syndrome
Family history of heart disease
High blood pressure
High LDL (bad cholesterol) and low HDL (good cholesterol)
Smoking
Obesity
Chronic stress
- Heart Arrhythmias
What It Is:
An arrhythmia refers to irregularities in the heart’s rhythm. The heart may beat too quickly (tachycardia), too slowly (bradycardia), or erratically.
Symptoms:
Fluttering in the chest
Dizziness or lightheadedness
Fainting spells
Chest discomfort
Causes:
Arrhythmias may arise independently or as a result of other heart conditions. Risk factors include:
Smoking
Excessive alcohol consumption
Obesity
Diabetes
Sleep apnea
Some types, such as atrial fibrillation (AFib), carry a heightened risk of stroke.
- Heart Failure
What It Is:
Heart failure means the heart isn’t pumping blood as efficiently as it should. It doesn’t mean the heart has stopped working entirely but that it’s too weak to meet the body’s demands.
Causes:
Long-term CAD
Cardiomyopathy (weakened heart muscle)
Thyroid disorders
High blood pressure
Symptoms:
Shortness of breath, even at rest or when lying down
Persistent fatigue
Swelling in legs, ankles, or feet
Chronic coughing or wheezing
- Heart Valve Disease
What It Is:
The heart contains four valves that control blood flow through its chambers. When a valve malfunctions—either by not opening properly or by leaking—it disrupts normal circulation.
Causes:
Congenital defects
Infections such as rheumatic fever or endocarditis
High blood pressure
Heart attack-related damage
Types:
Endocarditis: A bacterial infection of the valves, often treatable with antibiotics but potentially life-threatening without care.
Rheumatic Heart Disease: Long-term damage caused by rheumatic fever; less common today due to effective antibiotics.
Valve stenosis or regurgitation: Narrowing or leaking of valves, often requiring surgical repair or replacement.
- Pericardial Disease
What It Is:
Pericardial diseases affect the pericardium—the protective sac around the heart. The most common condition is pericarditis, or inflammation of the pericardium.
Causes:
Viral infections
Autoimmune disorders like lupus
Trauma or complications after heart surgery
- Cardiomyopathy
What It Is:
Cardiomyopathy involves changes in the heart muscle—such as thickening, stiffening, or weakening—that impair its ability to pump effectively.
Causes:
Genetic predispositions
Long-term high blood pressure
Viral infections
Alcohol or drug toxicity
Cancer treatments (chemotherapy)
Symptoms:
Difficulty breathing
Irregular heartbeat
Swollen extremities
Fatigue and weakness
- Congenital Heart Defects
What They Are:
These are heart abnormalities present from birth. They may be detected in infancy or remain unnoticed until adulthood.
Common Types:
Septal defects: Holes in the wall between heart chambers
Pulmonary stenosis: Narrowing of the valve to the lungs
Patent ductus arteriosus: A fetal blood vessel fails to close at birth
ALSO VISIT
Symptoms:
Blue or gray skin (cyanosis)
Breathing difficulties
Swelling around the eyes or limbs
Poor growth or fatigue in infants
Recognizing Heart Disease Symptoms
Symptoms vary depending on the specific condition but may overlap:
Condition Common Symptoms
CAD Chest pain, shortness of breath, pain in jaw or neck
Arrhythmias Chest fluttering, dizziness, fainting
Heart Failure Breathlessness, leg swelling, fatigue, cough
Valve Disease Chest discomfort, fainting, breathlessness
Cardiomyopathy Swollen feet, dizziness, fatigue
Congenital Defects Cyanosis, poor feeding or growth, fatigue
Diagnosing Heart Disease
Your healthcare provider will typically begin with a physical exam and detailed history. Depending on findings, several tests may follow:
Blood Tests: Evaluate cholesterol, blood sugar, and markers for heart inflammation or damage.
Chest X-ray: Checks heart size and fluid in the lungs.
Electrocardiogram (EKG): Tracks electrical activity of the heart.
Echocardiogram: Ultrasound images of heart structures and function.
Stress Tests: Measures heart response to exertion.
Cardiac Catheterization: A dye and X-ray procedure to view artery blockages.
Heart Disease Treatments
Treatment depends on the diagnosis but may include:
Lifestyle Changes:
Quit smoking
Adopt a heart-healthy diet
Engage in regular physical activity
Reduce alcohol and manage stress
Medications:
Blood pressure meds (e.g., beta-blockers, ACE inhibitors)
Cholesterol-lowering drugs (e.g., statins)
Anticoagulants or aspirin to prevent clots
Diuretics to reduce fluid retention
Surgical or Interventional Procedures:
Angioplasty and stenting to open blocked arteries
Valve repair or replacement
Bypass surgery
Heart transplant (in severe cases)
Cardiac Rehabilitation:
This program helps individuals recover after major cardiac events or surgeries and includes:
Supervised exercise
Nutrition education
Stress management
Support groups and counseling
How to Keep Your Heart Healthy
Whether or not you’ve been diagnosed with heart disease, adopting preventive habits is crucial:
Avoid smoking: It damages both heart and vessels.
Exercise regularly: Aim for at least 150 minutes of moderate activity weekly.
Eat a balanced diet: Focus on vegetables, fruits, lean protein, whole grains, and healthy fats.
Get enough rest: Most adults need 7+ hours per night.
Manage stress: Use techniques like meditation or yoga.
Schedule regular checkups: Monitor your blood pressure, cholesterol, and blood sugar.
Key Takeaways
Heart disease significantly impacts quality of life, but many forms are manageable with early detection and the right care. CAD remains the most common and dangerous form, but by working with your doctor and making heart-healthy lifestyle changes, you can reduce the risk or slow the progression of most heart conditions.
Frequently Asked Questions
Can I live a long life with heart disease?
Yes, many people do—especially with proper treatment and healthy habits. Advances in medication and surgery have dramatically improved survival rates.
What are early warning signs of heart disease?
The most common symptoms include chest pain and shortness of breath, particularly with exertion.
What happens after a diagnosis?
You’ll likely undergo more tests and work with a cardiologist to develop a treatment plan. Lifestyle adjustments, medications, and ongoing monitoring are key to long-term management.